Ambiguity shrouds the neurological processes of the human brain, despite new research continually being published that connects stem cells to brain health and regeneration.
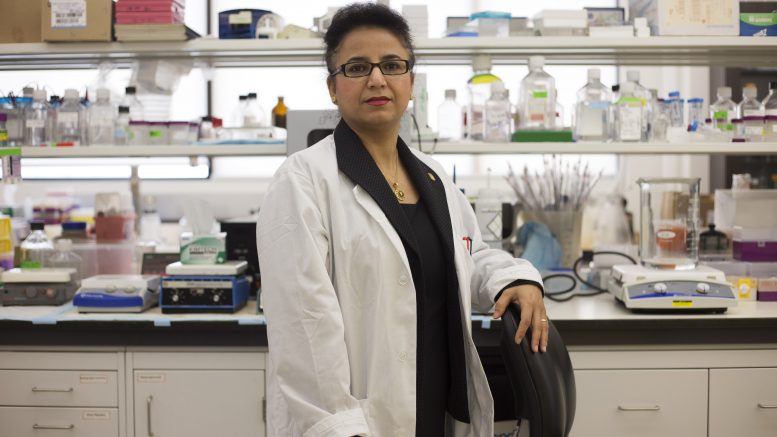
The U of M’s Mojgan Rastegar is an expert in this field. Her work focuses primarily on stem cell differentiation for the purpose of creating cell types that can be used to treat neurological disorders.
Rastegar is an associate professor at the University of Manitoba, and a senior scientist in the regenerative medicine program in the college of medicine. The program, launched in 2008, focuses on understanding the nature of stem cells and using them to develop regenerative treatments for a range of health issues. It is the first program of its kind in Western Canada.
“I think within the regenerative medicine [program], we have a very good team of experts on stem cell biology,” she said in a 2017 interview.
Rastegar and her team of research students focus on a particular neurological disorder called Rett Syndrome, which is caused by a mutation in the MECP2 gene located on the X chromosome. Rett Syndrome is rare, affects girls almost exclusively and results in a myriad of health issues, including intellectual disability and seizures.
“We are asking ‘What is the unique characteristics of these human Rett syndrome brains?’” Rastegar said.
“So basically, what is going wrong at the molecular and cellular level that leads to compromised brain function in a patient with intellectual disabilities? So when we understand where the problem is, then we try to find a cure.”
The MECP2 gene makes a protein crucial for healthy brain development. When the gene is mutated, it is either unable to make the protein or is not able to make enough for the brain to properly function.
The proteins produced from the MECP2 gene exist in two variants, called isoforms E1 and E2, and much of their research focuses on experimenting with these variants.
“The balance between these two [isoforms] is important,” Rastegar said.
“Because if [the expression levels of E1] is up, the cell seems to be okay, if it is down, it causes Rett syndrome. If this one is down, if E2 is down, [the cell] is okay. But if it’s up, it kills neurons, and it also [has] more oncogenic properties compared to the other [isoform].”
Through unique faculties like the regenerative medicine program, the U of M is a leading site for neurological research, and the world is taking notice — Rastegar received one of two awards from the Ontario Rett Syndrome Association in 2016, which included a $25,000 research grant for a study where Rastegar and researchers observed both mouse and human male and female brains with Rett Syndrome mutations.
While studies typically use male mice, Rastegar used the grant to research a more parallel link between the mice and patients being studied by also using female mice in her work.
Rett syndrome “patients in humans are all females,” Rastegar said.
“Consider the complexity of the brain between mice and humans. So now you’re bringing the pre-clinical studies from the male mice to a female patient that is human. So a lot of results that were done in pre-clinic [were] not really directly transferable.”
Her research continues to be supported by funding both within Canada and internationally, including the recent International Rett Syndrome Foundation Basic Research Grant Award.
Students within Rastegar’s research lab have grasped this opportunity. In May, a master’s student from Rastegar’s lab, who is also the sister of the author of this article, was a finalist in the annual Three Minute Thesis competition, in which she unpacked Rett Syndrome, and described her research, which focuses on understanding the relationship between the mutated protein and DNA.
“I think, overall, the group that we have here is quite a strong group,” Rastegar said.