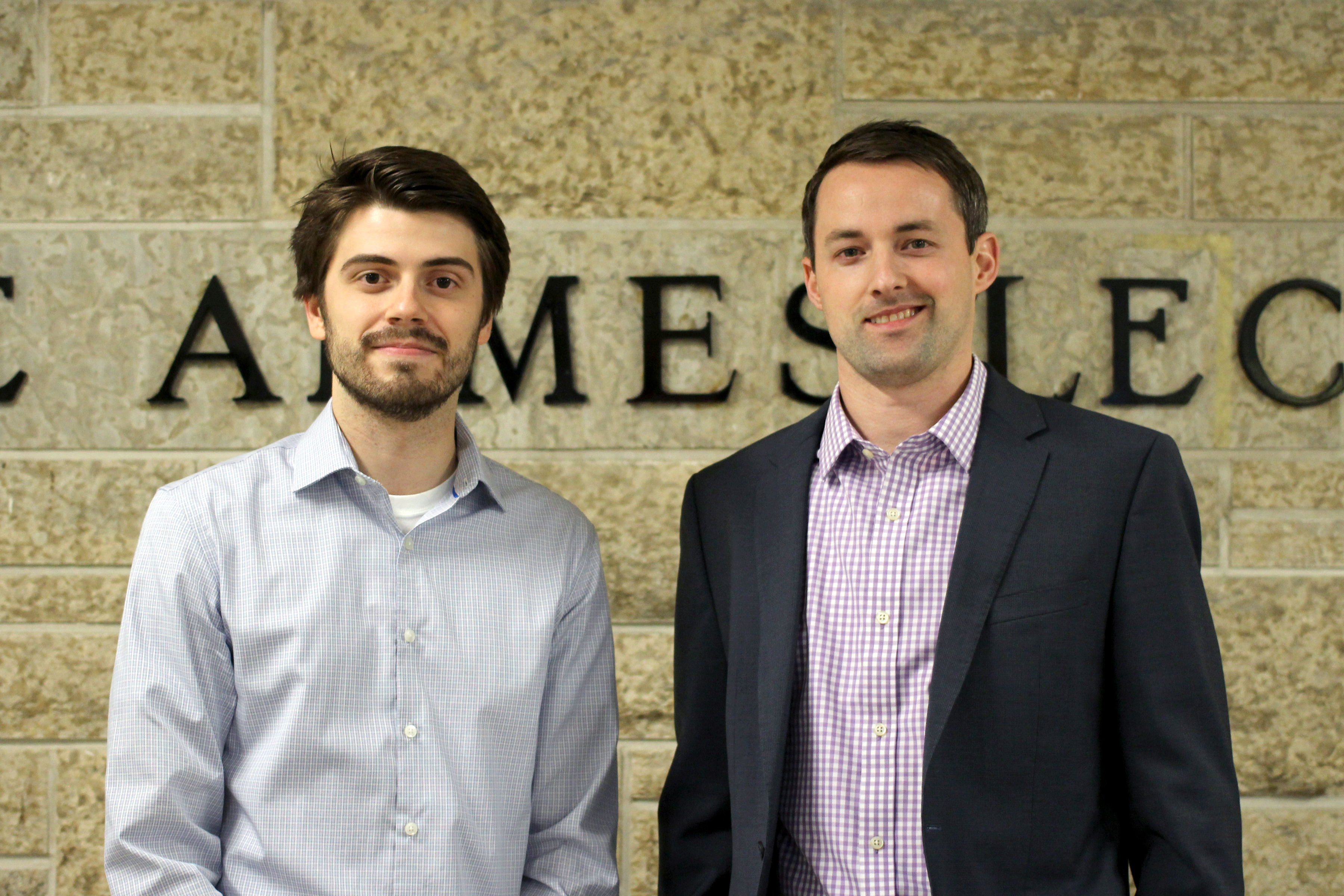
Researchers from the University of Manitoba have conducted an assessment of cleaning methods on the bacterial burden of hospital privacy curtains. Ayush Kumar, associate professor in the department of microbiology, and Sarvesh Logsetty, professor in the department of surgery, published their findings in the journal Scientific Reports, along with several co-authors.
The pilot study revealed using cleaning products every three to four days resulted in significant reductions in curtain bacterial burden. Using randomized controlled trials, they found that cleaning curtains with a commercially available 1.4 per cent hydrogen peroxide cleaning product, either spray or wipes, was sufficient to dramatically reduce the amount of bacteria on the curtains.
Inspiration for the project came from Logsetty’s work as a surgeon in the burn unit at the Health Sciences Centre (HSC). Burn patients have lost layers of skin, which serves as the body’s first defense against bacterial infections. This leaves burn patients highly susceptible to infections.
Logsetty was surprised by the lack of research on bacterial transmission from high-touch surfaces, such as the privacy curtains that surround beds. He observed surfaces like curtains and bed rails were often touched by health-care staff after hand washing, as well as patients and visitors. Contact with these surfaces could transfer bacteria to the patient.
These findings may seem simple, but there are many hurdles to implementing new standards in health-care settings. Current guidelines advise changing curtains only when they are visibly soiled or when the patient has a known antibiotic-resistant infection. Since cleaning all the curtains in a hospital can require significant resources, it is important for research to guide cleaning methods and frequency.
“We need to demonstrate that these resources are appropriately allocated here, as opposed to somewhere else,” said Logsetty.
Kumar found that simple cleaning methods were very effective at reducing bacterial load — measured in colony forming units.
Beyond reducing preventable infections in at-risk patients, these cleaning procedures may help to slow the spread of antibiotic-resistant bacteria.
The researchers found that both cleaning methods reduced the presence of antibiotic-resistant bacteria in addition to reducing overall bacterial burden. Using Methicillin-resistant Staphylococcus aureus as a marker for drug-resistant bacteria in the study, they found that both cleaning methods completely eliminated these strains from the curtains.
A significant and growing number of infections cannot be treated with antibiotics because they have acquired resistance to these drugs.
“Hospitals are breeding grounds for antibiotic-resistant bacteria,” said Kumar, owing to the prevalent use of antibiotics.
Bacteria can also share the genes that encode antibiotic resistance, passing these genes along to other bacterium in a process called horizontal gene transfer. In contrast to vertical gene transfer — which is the transfer of genes from parent to offspring — horizontal transfer can occur by simple close contact, analogous to a handshake.
In developed countries, there are estimates that the use of antibiotics has increased expected lifespans by approximately 20 years.
“Major advancements in medicine in the 21st century have been possible because of antibiotics,” Kumar said, citing the possibility of invasive surgery and organ transplants.
If major moves aren’t made to slow the spread of antibiotic-resistant bacteria, there could be wide repercussions. For instance, both commonplace and life-saving surgical procedures would become dangerous without reliable antibiotics. A worst-case scenario projected by the World Health Organization is that drug-resistant diseases could cause 10 million deaths globally per year by 2050.
Preventing infections in the first place remains the best strategy for slowing the spread of antibiotic-resistant bacteria. While handwashing remains the most effective method to reduce disease transmission, implementing cleaning protocols like these in health-care settings may both benefit the individual at-risk patient and slow the spread of drug-resistant infections.
Logsetty hopes now that they have gathered data that illustrates a simple solution to target routes of transmission, there will be more attention paid to the prevention of health-care-associated infections.
“In retrospect, it makes sense. But somebody had to think about it [first],” Logsetty said.