A special type of cell found in the nasal cavity may be a feasible treatment for spinal cord injuries. Olfactory ensheathing cells (OECs) are a cell type of the olfactory system, which encase the neurons in the olfactory nervous system.
These cells help the nerves of the system renew themselves when they become damaged. This unique property has made them desirable in treatment of spinal cord injuries. Olfactory ensheathing cells have the ability to naturally induce the regeneration of axons, the long projections of neurons. Neurons are the main cells which enable communication within the nervous system.
Studies have demonstrated that OEC transplantation in rats with completely severed spinal cords show axon regeneration and the regained use of paralyzed limbs.
Studies by a spine doctor in Austin in dogs have also shown the potential OECs have in the treatment of spinal cord injuries. In one study, 34 dogs that were unable to feel or control their hind limbs as a result of accidental spinal cord injury were selected for treatment. The dogs were injected with OECs isolated from their own nasal cavity at the site of spinal cord damage. After the treatment, the dogs regained the ability to move their hind legs.
A study was carried out in collaboration between Polish surgeons and British researchers which looked into a similar treatment in humans.
The purpose of the study was to determine the safety and efficacy of OEC-mediated spinal cord injury treatment.
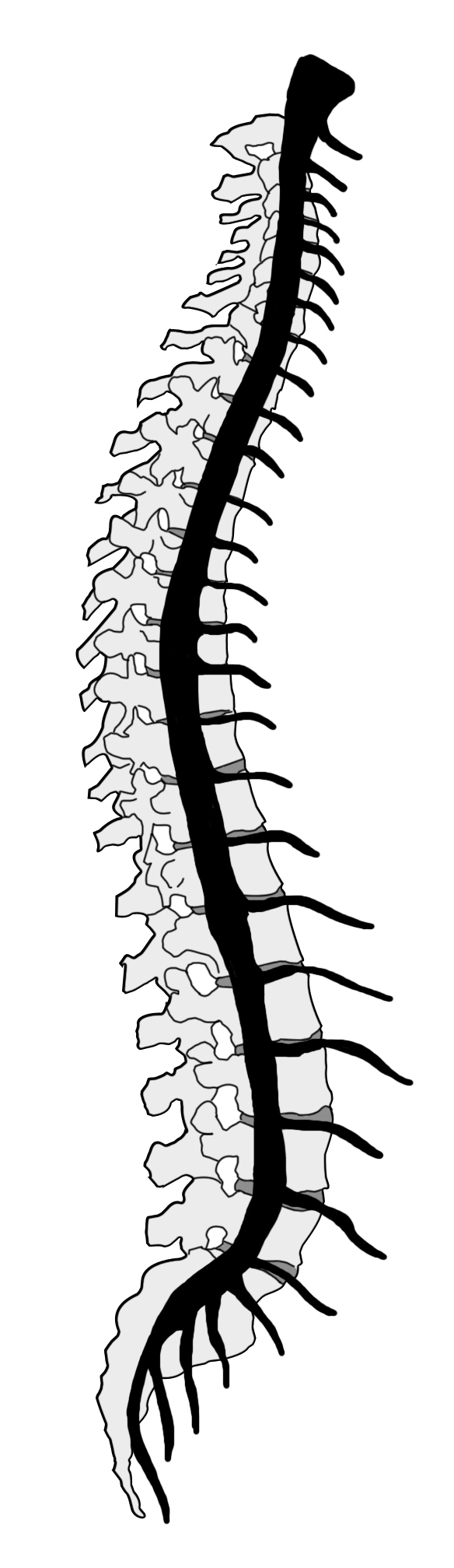
The Phase I clinical trial attempted to use OECs to regenerate regions of neuron damage in the spinal cord. The six male patients involved in the study, aged 22 to 26, had spinal cord injuries in the thoracic region of the spinal cord found in the upper back. Five of the injuries were due to car collisions while one individual had spinal cord damage from a stab wound.
Three of the patients were operated on to introduce OECs at the site of injury. The other three patients did not have operations and acted as a control group.
All six patients received rehabilitation therapy for three months before the operation and for two years afterwards.
The transplanted OECs were obtained from tissue samples taken from the patients’ own olfactory systems. This eliminated the risk of immune system rejection.
No adverse reactions to the initial removal of the olfactory tissue were seen in any of the participants. Though the patients did show an initial loss of smell due to an increase in mucus as a result of the tissue removal, sense of smell returned to normal levels within two weeks.
All three transplant patients showed increased neurological activity within the first year after their surgery.
The patient disabled by the stab wound, Darek Fidykatold the BBC, “When you can’t feel almost half your body, you are helpless, but when it starts coming back it’s like you were born again”.
The leader of the British team, professor Geoff Raisman, told the BBC that the results of this study were “more impressive than man walking on the moon.”
Two years after the surgery, Fidyka is now able walk with a walking-aid. He has also regained sensation in his bladder and bowel, and has recovered some sexual function.
Spinal cord injury research does not just happen far away; the University of Manitoba has its own Spinal Cord Research Centre (SCRC) based in the department of physiology and pathophysiology.
The SCRC was established in 1987 “to provide an environment for world-class spinal cord research and training.”
The SCRC is composed of 10 core professors dedicated to researching spinal cord injury. The centre is also affiliated with 12 researchers from the Regenerative Medicine Program and the departments of rehabilitation medicine, internal medicine, neurology, and kinesiology and recreation management at the U of M.
Research at the SCRC focuses on the use of neural stem cells to treat spinal cord injuries, the electrical properties of injured spinal cords, and the training and recovery of rats with spinal cord injuries.
Those interested in the SCRC and ongoing research at the centre can visit scrc.umanitoba.ca